Despite digital tools becoming standard, recording patient details continues to consume an increasing amount of time. What began as simple notes now shapes how services follow through, meet rules, receive payment, and account for decisions. Systems store information more easily today compared to ten years ago. Still, the load does not ease for doctors and their teams. Attention often shifts from people in front of them toward screens that require updates.
Among recent shifts in healthcare technology, linking AI medical scribes with EHR systems marks a fundamental change in record creation. Not mere voice-to-text devices, these systems act as smart intermediaries within clinical workflows. Proper setup allows the medical documentation platform to become an integral part of routine operations. This alignment enhances precision in patient notes while improving backend coordination. Over time, consistent use strengthens the reliability of stored health data. Some healthcare organizations now approach this challenge through tightly integrated clinical documentation systems, such as those developed by Himcos, where AI medical scribes function directly within established EHR workflows rather than alongside them.
Table of Contents
Understanding AI Medical Scribes within digital healthcare systems
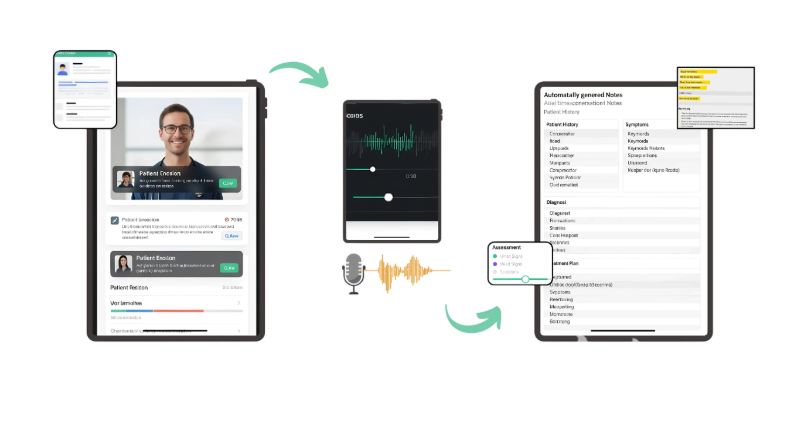
AI medical scribes operate using sophisticated language systems shaped by extensive exposure to clinical speech and specialized vocabulary. What emerges is more than mere transcription; these tools detect key health-related details during doctor-patient interactions. Because of this, records show structured reasoning around diagnosis, decisions about care direction, and upcoming steps instead of unfiltered talk. Not simply repeating phrases, they reshape conversations into coherent, purposeful summaries grounded in medical context.
When matched with EHR frameworks, such functions become meaningful in digital medical environments. How details are kept, accessed, reviewed, and transferred among treatment locations depends on these records. By linking dialogue-based inputs with organized patient files, AI scribes aid become sources of collective insight instead of isolated helpers.
Clinical context recognition in AI Scribe systems
Beginning with patient interactions, accurate understanding shapes how well an AI scribe functions. Spoken exchanges in healthcare often lack full sentences, including multiple speakers at once, while using terms unique to specific fields. Instead of treating words literally, these systems link utterances to medical ideas like observed conditions, identified illnesses, prescribed drugs, or intended treatments.
With access to EHR systems, contextual accuracy gains depth through alignment with past records, diagnosed conditions, or earlier consultations. Because of this linkage, consistency across time is easier to maintain, and redundant entries decline, especially when long-term patterns hold diagnostic weight.
Role of EHR systems in documentation architecture
From moment to moment, electronic health records function like the core network inside medical institutions. Across specialties, units, and timelines, they hold information about patients consistently, traceably, completely. These entries take shape through defined layouts, shaped less by preference than by rules tied to practice standards, compliance demands, and daily workflows.
How these systems store information changes when AI medical scribes connect directly. Left apart, outputs remain fixed as plain documents. When linked, records shift into dynamic inputs used for analysis, audits, or regulatory processes. The shape of upkeep alters based on connection status.
Structured data population and clinical continuity
Structured fields within EHR systems enable decision aids, performance tracking, because they follow standardized formats. When conversation becomes clinical data, integrated AI scribes assign precise codes matching those structures. These automated inputs fit schema requirements without manual re-entry. Translation occurs in real-time, guided by context rather than templates.
The data follows a consistent format, making it easier for those who deliver care later to review past records without difficulty. When information is organized this way, artificial intelligence used in medicine performs more reliably, especially when assessing group trends or forecasting outcomes.
Why integration determines operational value
Only when records move seamlessly into current platforms do efficiency gains appear. Without linking to EHR, AI medical scribes operate in isolation reducing overall effect.
Whether integration brings lighter documentation tasks or more reviews depends on clinician workflows. How smoothly later teams handle patient information hinges on these connections, shaping code precision, report speed, and preparedness for audits.
Workflow cohesion across clinical teams
When physician notes connect clearly to nursing logs, test results follow smoothly, along with paperwork details. Because of this link, pieces do not scatter needlessly through departments. Awareness stays steady among team members during patient handling.
Within standard EHR screens, AI scribes become visible immediately. Review happens during normal tasks, without disruption. Approval follows naturally, embedded in daily practice. Because the process fits existing habits, usage increases steadily. Responsibility remains clearly with the clinician at every step.
Technical foundations of AI scribe and EHR integration
Successful integration depends on system compatibility, data standards, and architectural governance. These elements determine scalability, performance stability, and long-term.
Through secure APIs, AI medical scribes connect to EHR systems, relying on standardized protocols for information transfer. Shaping how quickly they integrate, these underlying structures also affect long-term adaptability of clinical software environments.
Interoperability standards and data mapping.
Across healthcare systems, data flows through standardized formats like HL7 and FHIR, ensuring uniformity. With AI scribes aligned to these frameworks, entry into EHR becomes methodical. What emerges is seamless integration shaped by design precision.
When systems follow common standards, less time is spent building unique solutions. Compatibility among different EHR providers becomes easier to maintain. As a result, health organizations can update tools gradually. Changes in documentation methods are avoided during upgrades.
Clinical workflow evolution after integration
With integration comes shifts in how clinics operate ahead of, within, and beyond patient visits. As a result, attention patterns among providers shift, along with when records are updated and follow-up duties unfold. Prior routines give way to adjusted rhythms across the care cycle.
With AI medical scribes, notes happen nearer to patient encounters yet remain under clinician supervision. Effort spreads differently across tasks – workflow gains momentum even as record quality holds steady.
Pre-encounter context alignment
Integrated AI scribes pull scheduling details, patient background, and appointment type from the EHR prior to visits. Because of this, records capture purpose shaped by individual circumstances instead of standard forms.
Because context comes already aligned, fewer adjustments are needed after the visit. Note accuracy gains strength when past details stay connected, especially during recurring appointments. Chronic care benefits quietly through consistent background presence. Follow-ups gain precision without extra effort. What was documented before shapes what fits now.
Accuracy, governance, and clinical safety expectations
Every medical record must reflect exact details, clear origins, and correct adherence to standards. When systems connect, demands emerge for reliable information flow and structured oversight rules.
Supervised by clinicians, AI medical scribes assist while humans retain authority over final records. Built into EHR platforms, review processes help maintain necessary oversight during integration.
Auditability structures
With each update recorded, EHR systems log who made changes and when they occurred. Because AI-powered documentation tools follow these patterns, responsibility for patient data stays clear throughout care workflows.
Accountability structures
When clarity exists about which parts stem from AI versus physician review, legal standing improves during regulatory checks. Oversight becomes more straightforward where distinction is maintained between machine output and professional confirmation.
HIPAA compliance and data privacy considerations
Fulfilling requirements in health-related discussions means following data security rules without exception. When linked to electronic records platforms, AI medical scribes function under established protocols meant to safeguard personal medical details. Throughout the documentation lifecycle, rules shaped by HIPAA guide data capture, retention, and define access methods.

Secure data handling across systems
Secure transmission paths support AI scribes, while restricted entry rules limit usage. Within shielded systems, personal health details stay confined; compliance with medical safeguards guides their handling.
With role-defined permissions, access to documents remains limited to approved personnel. Confidentiality between clinical and administrative staff is preserved through structured user roles. Who views what depends on assigned responsibilities within the system.
Specialty-specific documentation expectations
Depending on the medical field, how patient information is recorded changes, shaped by unique goals, rules, and priorities. Systems using AI scribes adjust accordingly, matching the way data is captured to each specialty’s methods priorities. These tailored frameworks allow forms to stay organized without losing the detailed storytelling vital for diagnosis thought. Records become precise, fitting within institutional norms yet reflecting real-world specialist approaches.
Primary care and longitudinal documentation
Throughout primary care, notes cover prevention, ongoing health issues, one session after another. These records grow clearer when AI connects recent visits to past EHR files. Over time, consistent support helps organize treatment steps more effectively. Care pathways become clearer when transitions are managed without disruption. Long-term oversight benefits from steady communication between providers. Planning evolves smoothly when information flows continuously.
Impact on revenue cycle and coding processes
When documentation is clear, charges are more likely to reflect actual care. Because AI scribes record key clinical elements during visits, coded data tends to stay aligned with patient encounters. With documentation placed into organized EHR sections, coding staff face less back-and-forth; payment processing slows less often. Though clarity improves, timing shifts depend on system response.
Documentation completeness and financial clarity
When AI-produced notes match EHR requirements precisely, records become more complete; fewer gaps remain to affect coding precision or payment results. Because clinical data is gathered reliably, income flow becomes easier to anticipate, aiding departmental coordination behind the scenes. As record quality increases, financial operations grow more transparent within medical institutions; at the same time, care providers stay engaged with patients instead of being slowed by paperwork demands or process changes.
Organizational adoption and change management
Change unfolds gradually when clinical staff begin using AI-powered scribing tools. As habits shift, workflow structures adapt in parallel. Trust grows where record-keeping methods remain clear and consistent. Familiarity anchors the process, even amid technological updates. Integration within EHR systems keeps daily patterns intact. Cognitive load lessens under such conditions. Continuity supports acceptance over time. Professional responsibility stays visible throughout the transition. Smooth adaptation often follows when disruption is minimal.
Gradual trust emerges once AI-produced notes appear inside established EHR platforms, fitting naturally into standard record-keeping routines. Oversight becomes easier when clinicians see exactly how data enters the system. With each stable interaction, reliance grows not abruptly, but through steady reliability. Acceptance widens slowly among diverse team members as integration feels less disruptive over time.
Real-world implementation perspective
Now appearing in healthcare technology: real-world functionality matters more than promise. Companies like Himcos illustrate how AI medical scribes align with EHR workflows through structured integration approaches.
A leading provider of clinical documentation solution tools enables accurate recording of patient medical backgrounds under strict adherence to privacy regulations with HIPAA-compliant standards. Rather than deploying standalone infrastructures, these offerings ensure seamless alignment with current electronic health environments through organized data formatting.
Long-term evolution of integrated clinical AI
With progress in clinical AI, systems now handle more than just notes. Because of structured inputs, information feeds analysis. Quality tracking becomes possible when data flows correctly. Optimization in treatment paths follows from consistent details. From recorded interactions, integrated AI scribes extract patterns. These become organized inputs for long-term planning. Institutional insight grows through consistent data formatting. Strategic choices rely on such processed records. Clarity emerges when raw dialogue shifts into measurable form.
Documentation for health systems
Large healthcare systems gain measurable operational stability through standardised documentation practices supported by integrated AI scribes within electronic health record platforms. Because hospitals, clinics, and divisions follow consistent formats, information flows reliably making performance tracking both precise and repeatable. With expansion comes complexity; however, flexible integration approaches prevent overload on staff by maintaining structured processes. These systems stay manageable over time, shaped less by reactive fixes and more by overarching regulatory alignment.
What healthcare organizations should expect
Integrating AI medical scribes with EHR systems reshapes documentation as a clinical support function embedded within care delivery. Focus must shift toward seamless operations, organized information flow, regulatory preparedness, alongside clear gains in time management. While integration progresses, attention remains on how tasks align across systems. Efficiency metrics gain importance once setup completes.
One way some providers approach record keeping involves coordinated systems, like those offered by Himcos, using automated transcription that fits within existing patient summary workflows alongside protected information management. In such setups, AI medical scribe assist note creation over time without replacing physician review or compliance requirements.