Finding the true (Electronic Health Records) EHR Implementation cost is dependent on ‘n’ number of factors. If you are a healthcare provider thinking about switching to the electronic health record (EHR) system, then there is a likely question: how are we going to pay for it? The shift from the paper chart in a digital system promises better patient care and streamlined operations, but the costs are upfront and running feels hard without a clear plan. From software and hardware to training and maintenance, EHR implementation is a major investment. But it is also one that can pay in efficiency, accuracy and happy patients. In this guide, we will break the actual costs of EHR implementation, share strategies to keep your budget in check, and highlight the financial victory you can expect below the road. Let’s dive!
Table of Contents
What is EHR, and why does it matter?
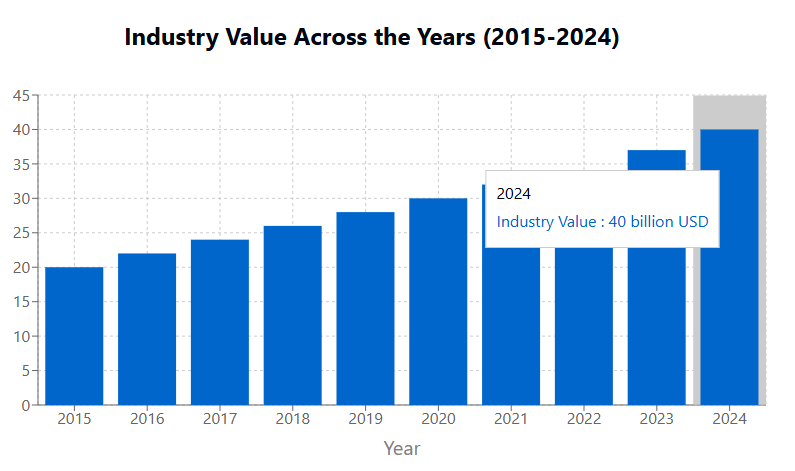
An Electronic Health Record (EHR) is a digital platform designed to store and manage the patient’s information by replacing traditional paper-based records. It enables real -time access to important medical data, eventually enhances the quality of patient care and streamlines clinical operations. The cost of implementing the EHR system includes several factors including software and hardware investment, staff training, data migration and ongoing system maintenance. While initial investment may seem more, many healthcare providers adopt membership-based pricing models to manage costs efficiently. Beyond financial ideas, EHRs help improve operating efficiency, reduce errors and support better healthcare distribution. Below is a detailed observation of EHR implementation expenditure.

EHR Implementation Cost Breakdown
EHR implementation costs vary depending on the organization’s size, system complexity, and specific customization requirements. Below is a detailed breakdown:
1. Direct cost: software licensing and adaptation
The cost of EHR software varies on the basis whether a healthcare provider selects an off-the-shelf solution or custom-made system. Pre-paired EHRs usually come up with a repayor or per-facility pricing. The repatriate model, the cost of $ 100 to $ 150 per user, is suitable for small practices, but becomes expensive for large outfits. Meanwhile, the per-convenient model, from $ 1,000 to $ 10,000 per month, provides better scalability for large hospitals. Custom EHR, suiting specific operating requirements, provide better integration and flexibility, but falls at a high price, usually between $ 500,000 and $ 700,000 for medium -sized hospitals. It is necessary to choose the right pricing model for long -term financial stability.
2. Hardware Investment: Infrastructure and Equipment
Hardware cost is an important part of EHR implementation, depending on the size of healthcare facility and the needs of infrastructure. Large hospitals usually require server, networking hardware, and advanced computing systems to support high patient versions and data security, which costs more than $ 100,000. Small practices reduce expenditure by adopting cloud-based EHR solutions, which limit hardware dependence. In such cases, the cost usually ranges from $ 10,000 to $ 100,000+, which is based on the required upgradation. Proper, invested in high-demonstration hardware prevents uninterrupted EHR functionality, protecting the patient data, and downtime-related disabilities that disrupt clinical operations, eventually affect patient care and workflow efficiency.
3. Implementation Services: Setup and Adaptation Support
A successful EHR rollout requires professional support from project managers, IT experts, advisors and trainers to align the system with an organization’s workflow. The pre-constructed EHR system often has minimal setup requirements, making the implementation easy and less expensive. However, custom-made solutions require detailed configurations, workflow integration and training of employees, which significantly increase the expenditure. Healthcare organizations usually allocate 15–20% of their EHR budget for implementation services, ensuring a smooth system. These services also include troubleshooting, technical aid and adaptation strategies, which help organizations originally infect, reduce operational downtime, and to maximize long -term EHR efficiency, maintaining compliance with industry rules.
4. Indirect Cost: Downtime and System Maintenance
Beyond direct expenses, the EHR implementation reduces hidden costs, including downtime, productivity loss and system maintenance. Paper records or heritage systems disrupt daily operations, leading to short -term workflow inability. Additionally, regular systems upgrade, safety patch and module expansion require ongoing investment. The cost of first year maintenance costs from $ 10,000 to $ 50,000, usually depending on the system complexity. However, these expenses decrease over time as employees become skilled in using EHR. Investing in ongoing support and software updates ensures long -term efficiency, compliance with system safety and developing healthcare rules, eventually increasing patient care and operational continuity.
5. Workforce Costs: Training and Labor Expenditure
Staff training is an important aspect of EHR implementation, as effective adoption reduces errors and improves system purposes. Larger hospitals with many departments and complex workflow require extensive training, which costs much higher than in small clinics. Early training expenses typically range from $ 1,000 to $ 5,000 per staff member, including workshops on hands, webinars and training manuals. Additionally, ongoing training is necessary to adapt to the system updates and new features, the cost of $ 500 and $ 2,000 per staff member per staff. Investing in comprehensive training ensures that health professionals maximize EHR efficiency, streamline workflows, and increase the patient’s safety by reducing the risk of medical errors.
What further affects the price tag?
Beyond these main costs, other factors move the total. The deployment model you choose plays a big role. The on-rims system, hosted on its own server, requires a heavy upfront investment-even at the same time from $ 1,000 to $ 500,000 as well as hardware and support spending. In contrast, cloud-based options, run on $ 200 to $35,000 monthly membership plans, offer flexibility without large hardware hits. Integrating your EHR with the existing tool, such as telemedicine platform or lab systems, everything coincides to work together, adding another layer of expenses for APIs and testing. Then there are hidden costs such as data migration – the old record roles in the new system – which differ based on data volume and complexity, and compliance, which ensures that you meet rules like HIPAA or GDPR with additional training or safety measures.
Unseen expenses affecting EHR implementation
1. Data Transfer
The patient’s record and clinical information from the legacy system requires accuracy to maintain accuracy and efficiency to move to a new EHR. This process demands special tools and expert assistance to ensure a spontaneous transition. Certified EHR helps professional tailor solutions and see transfer effectively. The cost associated with data migration depends on factors such as data volumes, complexity and format variations.
2. Regulatory Compliance
It is important to comply with standards such as HIPPA, FDA, and more to protect the patient’s information and ensure responsible electronic health record management. Getting compliance may include exposure assessment, implementing encryption, implementing training staff and maintaining audit logs. Costs are rapidly ups and downs depending on organizational requirements. Choosing software with full HIPAA compliance helps maintain safe and efficient patient care.
Cost effective strategies for EHR implementation
Adopting the EHR system greatly improve healthcare operations, but the implementation process requires careful planning and resource management. Here are some strategies to ensure a smooth and cost-skilled transition.
1. Choosing a reliable software vendor
It is important to select the right EHR provider for a successful implementation. Look for sellers that provide adaptable and scalable solutions to suit your practice needs. A flexible system that basically integrates with existing workflows prevents expensive disabilities. Additionally, partnership with an experienced seller familiar with healthcare rules such as HIPAA compliance, ensures long -term stability and reduces the risk of compliance issues.
2. Using Open-Sound Library
Open-sources solutions provide an effective way to control EHR implementation expenses. These systems offer flexibility, allowing healthcare providers to revise the software to meet their requirements to avoid expensive licensing fees. However, organizations should evaluate their ability to manage, adapt and maintain open-source software, considering factors such as technical expertise, integration with existing systems and regulatory compliance. When properly executed, this approach helps reduce both initial investment and long -term costs, especially beneficial for small health care features.
3. Applying a minimum viable product (MVP)
A phased implementation approach cuts the cost. Launching with an MVP that contains only the required features ensures a sharp, more cost-efficient rollout. This method reduces initial expenses by allowing providers to assess the user’s response and refine the system before expanding their functionality. Preference to important components helps maintain workflow continuity and adopt the user.
4. Priority to safety within the budget plan
Strong safety measures are necessary for the protection of patient data in any EHR system. Facilities such as role-based access control (RBAC), encryption, automatic session timeout, and regulatory standards should be integrated into the implementation scheme. Cooperating with vendors who specialize in safe healthcare technologies, help reduce risks when optimizing costs. While safety investment increases advance expenses, they prevent data violations that cause significant financial and reputed damage.
The Payoff
Financial Benefits of EHR EHRS is not just a cost – they are a revenue booster over time. They improve billing accuracy, accelerate reimbursement and reduce revenue leaks, with a study showing a strong return on investment within a few years. By automating tasks such as scheduling and paperwork, they cut in administrative time, making employees focus on patients. In addition, patient data leads to quick access to smart decisions, less complications and low reading costs. For example, a clinic using the integrated billing saw low errors and rapid payment – stops giving evidence of the expenses.
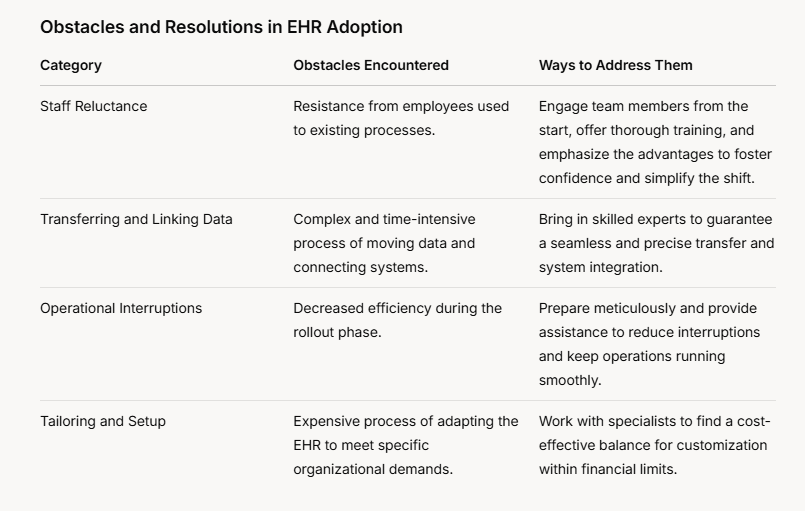
Challenges (and improves) you might face
No major change is easy, but knowing the obstacles helps. Employees oppose proceeding from familiar workflows, so include them quickly and offer training that highlights the benefits to win them. Data migration is difficult and time-consuming, but hiring professionals who pulled a zero-downtime migration for OC Sports-Easer accuracy. Workflow disintegration dent productivity at the first time, so plan well and bend at the seller’s support to keep things stable. Customs are expensive, but cleverly maintains it within the budget to work with experts.
How does Himcos helps?
Himcos builds cloud-native, AI-powered software solutions to transform clinical and financial data into actionable insights. Jump from setup to success in days with our specialized workflow solutions for different healthcare settings. We deliver innovation within a planned financial framework for maximum value in every development sprint. Our platform grows alongside your healthcare institution, with features designed to expand with operations.



